OPINION:
In 2017, my friend Toni Brown was expecting her family’s first grandchild. What should have been one of the happiest days of their lives quickly turned into one of the worst, as Toni and her family were informed that delivery complications had left her daughter in a coma. Toni’s daughter tragically died a few days later, and her doctors were not able to give her family a clear answer about what caused the young mother’s complications and untimely death.
Toni’s story is heartbreaking but unfortunately not unique.
In the United States, there are an estimated 700 pregnancy-related deaths per year, 60% are considered preventable. The crisis is most severe for Black mothers in America, who are dying at three to four times the rate of their white counterparts.
The maternal health crisis cuts across class, education, and income to disproportionately kill Black women. Celebrities such as Serena Williams, Allyson Felix, and Beyonce have experienced severe pregnancy-related complications.
There are many factors contributing to the increased impact of the maternal health crisis on Black women, including lack of access to healthcare, affordability of care, bias among healthcare providers, and certain pre-existing conditions which impact Black women at a higher rate than other women.
Additionally, we know that lupus, sickle cell disease, hemorrhage, and hypertensive disorders are leading causes of maternal mortality and severe morbidity. These conditions and others such as mental health conditions disproportionately impact Black women, and we need improved training of our healthcare professionals to identify and treat these conditions throughout pregnancy and the postpartum period.
This is also an issue that has serious impacts on women living in rural areas. Access to care is limited: from 2010-2019, 100 rural hospitals closed their doors and of those that remain, 20% are at risk of closing. Additionally, 54% of rural hospitals lack obstetrics units altogether.
This crisis will not disappear without federal action. We must pass legislation to improve training within our healthcare system and increase resources for pregnant and postpartum women of color.
I invited Toni to join me and speak at the White House’s first ever Maternal Health Day of Action, which Vice President Harris hosted in December. We discussed many of the necessary improvements needed in our healthcare system to improve maternal health outcomes for Black women. One of those solutions was passing my bipartisan Maternal Health Quality Improvement Act (MHQIA).
I’m thrilled that this legislation was recently passed as part of the FY22 Omnibus Appropriations. This will authorize grant programs to improve maternal health outcomes by developing evidence-based best practices, improve maternal mortality review committee data, evaluate new models of care, and address bias training for health care providers.
This legislation will also authorize a grant program for developing integrated health care services for pregnant and postpartum women and infants. This has consistently been recommended by experts as a solution for reaching populations who lack health insurance or access to regular healthcare checkups.
Integrated care will treat mothers more holistically and coordinate services between mental health, social services, substance use disorder treatment and maternal health. Even when new moms lack coverage to visit a doctor themselves, they continue taking their baby to appointments. These appointments are an excellent opportunity for healthcare professionals to ensure that mothers are recovering from childbirth.
In addition to killing our mothers, the maternal health crisis is costing our healthcare system billions of dollars each year. The Commonwealth Fund recently released a report listing the estimated total maternal morbidity costs for all U.S. births in 2019 to be $32.3 billion from conception through the child’s fifth birthday. The largest costs included maternal mental health conditions ($18.1 billion), hypertensive disorders ($7.5 billion), gestational diabetes ($4.8 billion), and postpartum hemorrhage ($1.8 billion).
Those economic and human costs are part of the reason the Maternal Health Quality Improvement Act is a solution to the maternal mortality crisis that is supported on both sides of the aisle. Maternal mortality and severe maternal morbidity are devastating families and eviscerating hospital budgets.
This is an issue I have worked to eliminate since coming to Congress in 2013. I am proud that this bill contains major provisions from my MOMMA’s Act. We must act now. Implementing solutions like those outlined in my Maternal Health Quality Improvement Act will cut costs for our healthcare system and save the lives of mommas and babies so that stories like my friend Toni’s never happen again.
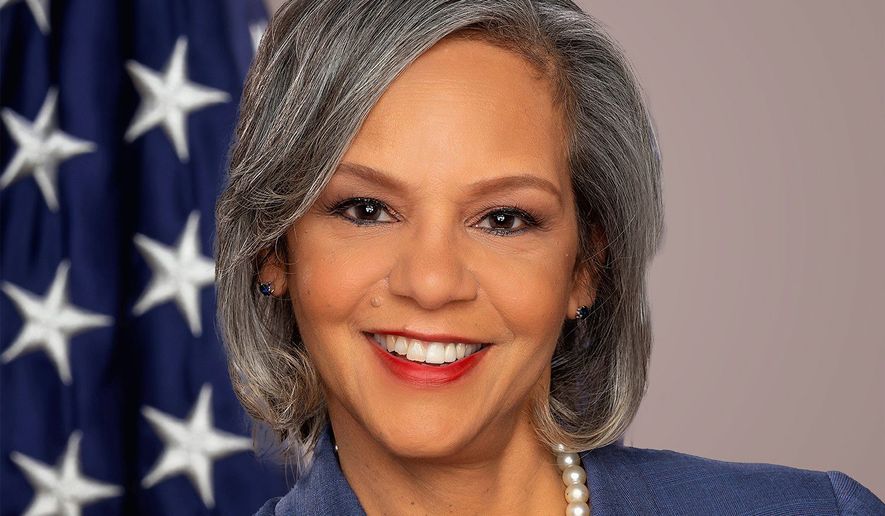
• Dr. Robin Kelly, Illinois Democrat, is Chair of the Congressional Black Caucus Health Braintrust and Vice Chair of the House Energy and Commerce Committee. She represents the 2nd Congressional District and has been a leading voice in Congress on the maternal health crisis since 2013.



Please read our comment policy before commenting.