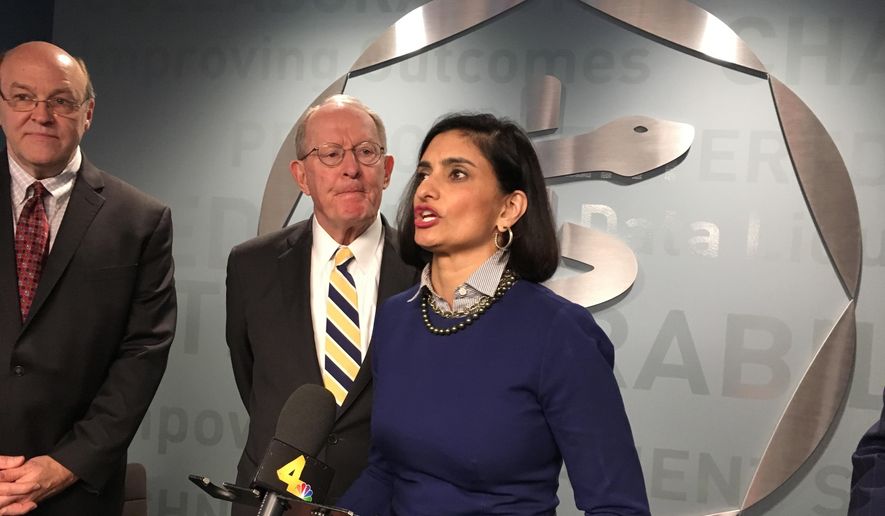
A Senate panel scrutinizing Medicaid overpayments says the administration’s push to audit states more closely is good news but that it needs to hear more from Seema Verma, who oversees the program but did not testify alongside government watchdogs on Wednesday.
Sen. Heidi Heitkamp, North Dakota Democrat, said “time’s a-wastin’ ” as they seek details from the Centers for Medicare and Services, which oversees the federal-state insurance program for the poor but has struggled for years to rein in bogus payments.
“I want a plan, and I want it sooner rather than later,” said Ms. Heitkamp, who supported Ms. Verma’s confirmation last year and faces a tough re-election battle in a red state this fall.
Improper payments soared from $14.4 billion in 2013, the year before Obamacare’s expansion of the program, to $37 billion in 2017, meaning Medicaid accounts for roughly a quarter all improper payments in the federal government, according to the Homeland Security and Governmental Affairs Committee.
“We are spending hundreds of billions of dollars — we want this money spent well,” committee Chairman Ron Johnson, Wisconsin Republican, said.
CMS said this week it will clamp down on improper payments as part of its broader overhaul of the Medicaid program, which lets states impose work requirements on able-bodied recipients and resulted in a web-based “scorecard” of health outcomes in reporting states.
Yet Democrats fumed over the lack of testimony from Ms. Verma, saying she should have paired a Tuesday press release about agency efforts with testimony at Wednesday’s hearing.
“Is there a reason why she’s not here today?” Ms. Heitkamp said.
“I just don’t think she was prepared,” Mr. Johnson said, though later said it is early in the oversight process, so it made sense to hear from government inspectors and get a progress report from Ms. Verma later on.
“She’s happy to come whenever we do a follow-up hearing on this,” he said. “She’s more than willing to testify.”
For its part, CMS said the administrator was unable to match her schedule with the hearing date, though Ms. Verma takes the issue seriously and will work with the committee.
The agency said it will begin auditing states with a track record of eligibility errors, to ensure that people aren’t accepting beneficiaries who don’t actually qualify for the legacy Medicaid program or its expansion population under Obamacare.
States are responsible for determining if people are eligible, and that creates an opening for bad payments since CMS hasn’t performed comprehensive audits of those decisions. For instance, states might fail to verify a recipient’s immigration status.
CMS said it will scrutinize how much money is spent on actual care, versus administrative costs, and demand complete and accurate data from states. It will also educate doctors on ways to avoid billing errors, and expose states that underperform on its newly created Medicaid “scorecard.”
Medicaid is the federal-state partnership to provide health coverage for the poor. Created as part of the Great
Society programs of the 1960s, it has steadily increased in size to cover 70 million people at a cost of $554 billion a year — most of that from federal taxpayers.
The program saw a major expansion under Obamacare, with the federal government trying to entice more poor people to sign up by expanding eligibility to families that make above 100 percent of the poverty level. Most states have signed on board the expansion, accepting a generous federal match in exchange for promising to pick up more of the tab themselves in the future.
“With historic growth in Medicaid comes an urgent federal responsibility to ensure sound fiscal stewardship and oversight of the program,” Ms. Verma said Tuesday.
Her program-integrity plan dropped several days after Mr. Johnson released a report saying CMS doesn’t have an anti-fraud strategy, and has ignored 11 separate recommendations by the Government Accountability Office over the last three years to combat fraud.
Brian Ritchie, assistant inspector general at the Health and Human Services Department, said CMS’s outline is a “step in a positive direction” but “more details need to be there.”
“They have a big effort underway in order to [correct things], but it’s got to be done properly,” GAO Comptroller Eugene Dodaro said.
Mr. Dodaro said CMS should do what it can to help state-level auditors, who “know this program better than anybody.”
“If they are given proper support and resources, you can prevent a lot of these program-integrity problems,” he said.
• Tom Howell Jr. can be reached at thowell@washingtontimes.com.



Please read our comment policy before commenting.