Twitter is grand fun, Facebook can be useful and informational, and all sorts of computer activities have become second nature to most of us. However, one thing you will not find in my office is electronic medical records (EMR).
My reasons are many, including concerns about the security of sensitive information, cost, loss in efficiency estimated to be 20 percent, and potential degradation of the sanctity of the doctor-patient relationship. Now, I am being punished by the Center for Medicare and Medicaid Services (CMS) for my non-compliance with government-mandated EMRs and certain nonsensical reporting with a 5 percent reduction in payments for services provided to my Medicare patients in 2015.
Medicare and Medicaid have served as the template for Obamacare and government-controlled medicine. This began with price controls on doctors and hospitals resulting in cost-shifting to the private sector and spiraling health care costs. Politicians used this predictable outcome to clamor for healthcare overhaul. The crucial cost-control piece in the final implementation of Obamacare is the centrally connected EMR database. It is to be the vehicle by which the patients’ conditions are monitored and their treatment options elucidated based on centrally determined “best practices” and factors such as age and pre-existing pathology.
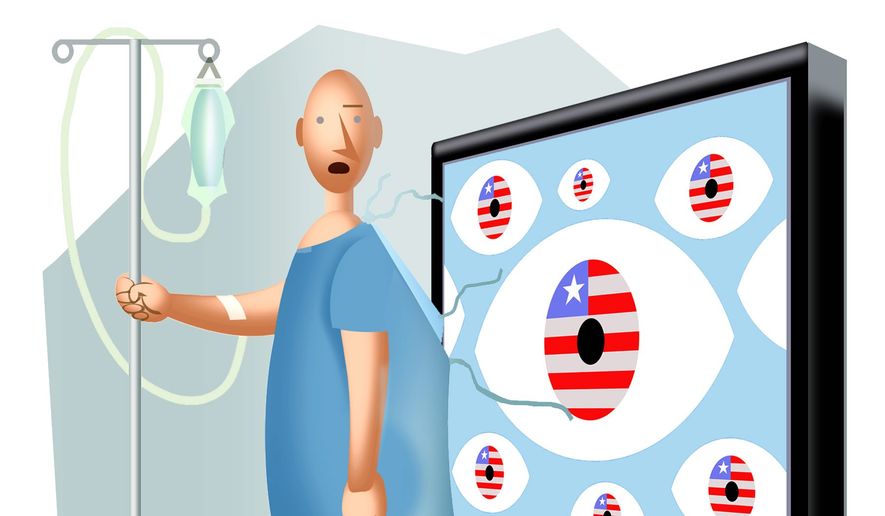
Physician compliance with recommended treatments will be monitored and corrected when necessary. People the likes of Jonathan Gruber and Ezekiel Emmanuel will be deciding these parameters as appointees to the Council for Comparative Effectiveness Research and the Independent Payment Advisory Board (IPAB).
By its own admission, the federal government plans on sharing your collected data with approximately 35 agencies to “improve health care.” These include the IRS, Department of Defense, the Agriculture Department, Homeland Security, Health and Human Services, CMS, etc. Welcome to the age of “population health,” World Health Organization international codes, “health justice” and the end of individualized healthcare decisions. When this is understood, the actions by the CMS to incentivize physicians to adopt EMR become clear. Even more importantly, they become a template for understanding how bureaucrats with all of the power of the government behind them operate.
Initially, CMS offered physicians and hospitals cash incentives to adopt EMR. Computer companies and IT groups sold physicians and hospitals on the idea that EMR could be programmed to withstand any payment audits and to support the level of charges billed to any insurance entity. Once providers adopted the EMR, the next phase was new CMS mandates that “meaningful use” reports be filed to prove government criteria were being met. Phase 1 was fairly basic. However, phase 2 — meaningful use criteria — are much more time-consuming and costly. Only 2 percent of physicians have met them, and failure to meet them results in penalties.
Recently, CMS has hired a company to randomly audit 10 percent of providers who received money for EMR for possible recoupment if they failed to fully comply with MU 1 or 2. Now imagine the impact on your healthcare with the threat of future recoupment of payments if your physician fails to follow the CMS-mandated guidelines for care. These will come when the cost of healthcare exceeds government resources. (Think IPAB).
You might be asking how this degrades the sanctity of the doctor-patient relationship. In view of the recent spectacular data breaches in government and private entities, the safety of the individual’s health and personal status as well as financial data in the medical record is potentially not secure.
This means that the patient may be reluctant to discuss crucial but sensitive information with his physician, not to mention the physician’s reluctance to enter it into the record. Further, the physician’s ability to craft a treatment plan specific to that individual may be hindered by the treatment templates envisioned by the central planners utilizing the EMR for conveyance. The 20 percent decrease in productivity means decreased capacity to take necessary time with patients. Ultimately, with the subsidized Obamacare insurance added to the Medicare and Medicaid government expenditures, the Independent Payment Advisory Board will decide what treatments, drugs and visits are cost-effective and approved for payment. In other words, rationed care. And how will care be rationed? It will be through the EMR data entered by the physician on his or her patients.
Those of us who have read the ACA and analyzed our healthcare system with an eye towards effective reform, realize that Obamacare is not feasible as designed. Great Britain finally gave up trying to centralize their EMR after 20 years. Our own Department of Defense failed after 10 years to interconnect its computer system with the VA System. In my own practice, I have several physician patients who have retired over EMR conversion and its disruption to personalized patient care. Several have gone back to paper charts after spending thousands of dollars to computerize. Some physicians enjoy their EMR but have no plans to centrally connect them to government agencies.
When we have a government forcing us to buy insurance products we don’t want with narrow networks and high deductibles we can’t afford, or government-approved EMR which reduces productivity and compromises the sanctity of the doctor-patient relationship, we are not the land of the free. When we continue to tolerate the army of Gruberite bureaucrats interfering with the unfettered practice of quality medicine, or our access to the physicians of our choosing, or affordable healthcare plans that fit our family’s needs, we are not the home of the brave.
Jane Lindell Hughes, M.D., F.A.C.S., is a board certified ophthalmologist in private practice and is a clinical professor in the department of ophthalmology at the University of Texas Health Science Center in San Antonio.



Please read our comment policy before commenting.